New Study Finds Resolvin E1 is a Pro-repair Molecule that Promotes Intestinal Epithelial Wound Healing
By Elizabeth Walker | April 14 2020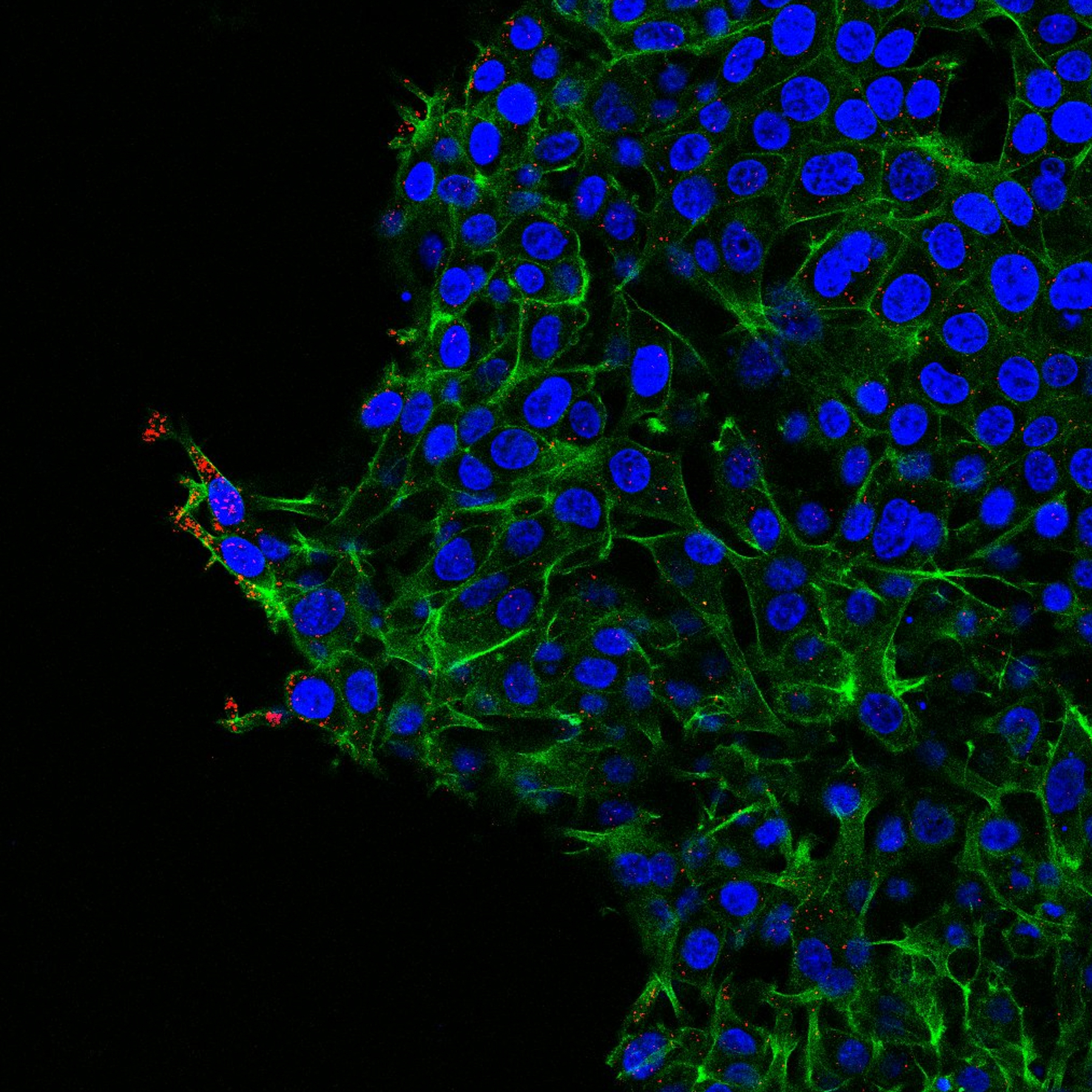 Resolvin E1 (RvE1), a lipid derived from Omega-3 fatty acids, is a pro-repair molecule that promotes healing of intestinal wounds according to a recent study published in PNAS as a collaborative project between The Department of Pathology at the University of Michigan Medical School and the George W. Woodruff School of Mechanical Engineering and the Petit Institute for Bioengineering and Bioscience, Georgia Institute of Technology.
Resolvin E1 (RvE1), a lipid derived from Omega-3 fatty acids, is a pro-repair molecule that promotes healing of intestinal wounds according to a recent study published in PNAS as a collaborative project between The Department of Pathology at the University of Michigan Medical School and the George W. Woodruff School of Mechanical Engineering and the Petit Institute for Bioengineering and Bioscience, Georgia Institute of Technology.
RvE1 is a member of a family of molecules known as specialized pro-resolving mediators, which help in the recovery from inflammatory processes. Numerous articles describe how RvE1 promotes resolution of inflammation by actively facilitating clearance of immune cells, but the mechanisms of how RvE1 promotes tissue repair are still elusive. This study identifies pro-repair effects of RvE1 on intestinal epithelial cells.
Intestinal epithelial cells function as a critical barrier that separates luminal contents containing bacteria from underlying mucosal tissues. Injury or wounds to the epithelial barrier can therefore have detrimental effects due to release of luminal bacteria into the mucosa, resulting in an inflammatory response. Thus, repair of epithelial wounds is vital for restoring intestinal barrier and preventing unwanted exposure to external agents in the gut lumen.
In response to injury, intestinal epithelial cells migrate and divide to cover exposed surfaces, repair wounds, and restore barrier. In this study, the authors demonstrate that RvE1 increases the repair properties of intestinal epithelial cells, both in cultured human cells and in injured murine colon tissues.
 “The delicate balance of inflammation, resolution and repair is perturbed in chronic inflammatory diseases such as inflammatory bowel disease (IBD), a condition associated with uncontrolled inflammation and epithelial wounds,” says Asma Nusrat, MD, professor and director of experimental pathology at the University of Michigan Medical School. Nusrat was the lead author of the study.
“The delicate balance of inflammation, resolution and repair is perturbed in chronic inflammatory diseases such as inflammatory bowel disease (IBD), a condition associated with uncontrolled inflammation and epithelial wounds,” says Asma Nusrat, MD, professor and director of experimental pathology at the University of Michigan Medical School. Nusrat was the lead author of the study.
“Thus, mediators that influence both resolution of inflammation as well as restore epithelial barrier properties are valuable candidate therapeutic agents for these conditions,” Nusrat adds.
An additional important aspect of this study is the generation and delivery of RvE1 in nanoparticles, which had potent pro-repair effects on the healing of colonic wounds.
“We developed nanoparticles that target the delivery of RvE1 to sites of injury and control the release and stability of the molecule, increasing its repair abilities,” says co-author and biomaterials expert Andrés García, PhD, a Regents’ professor at Georgia Tech, where he is executive director of the Petit Institute. “The engineering of biomaterials to control delivery of these potent molecules is an important step in developing therapeutic applications for patients.”
Some of the current therapies available for IBD treatment are immunosuppressive drugs meaning that while they decrease inflammation, they also turn the patients into moving targets for opportunistic infections.
 “Our findings are potentially important to IBD patients as RvE1 seems to be an immunoresolvent agent capable of decreasing inflammation and increasing intestinal mucosal repair without compromising the patient’s immune response,” explains U-M Pathology's Research Investigator Miguel Quiros, PhD, first author on the paper.
“Our findings are potentially important to IBD patients as RvE1 seems to be an immunoresolvent agent capable of decreasing inflammation and increasing intestinal mucosal repair without compromising the patient’s immune response,” explains U-M Pathology's Research Investigator Miguel Quiros, PhD, first author on the paper.
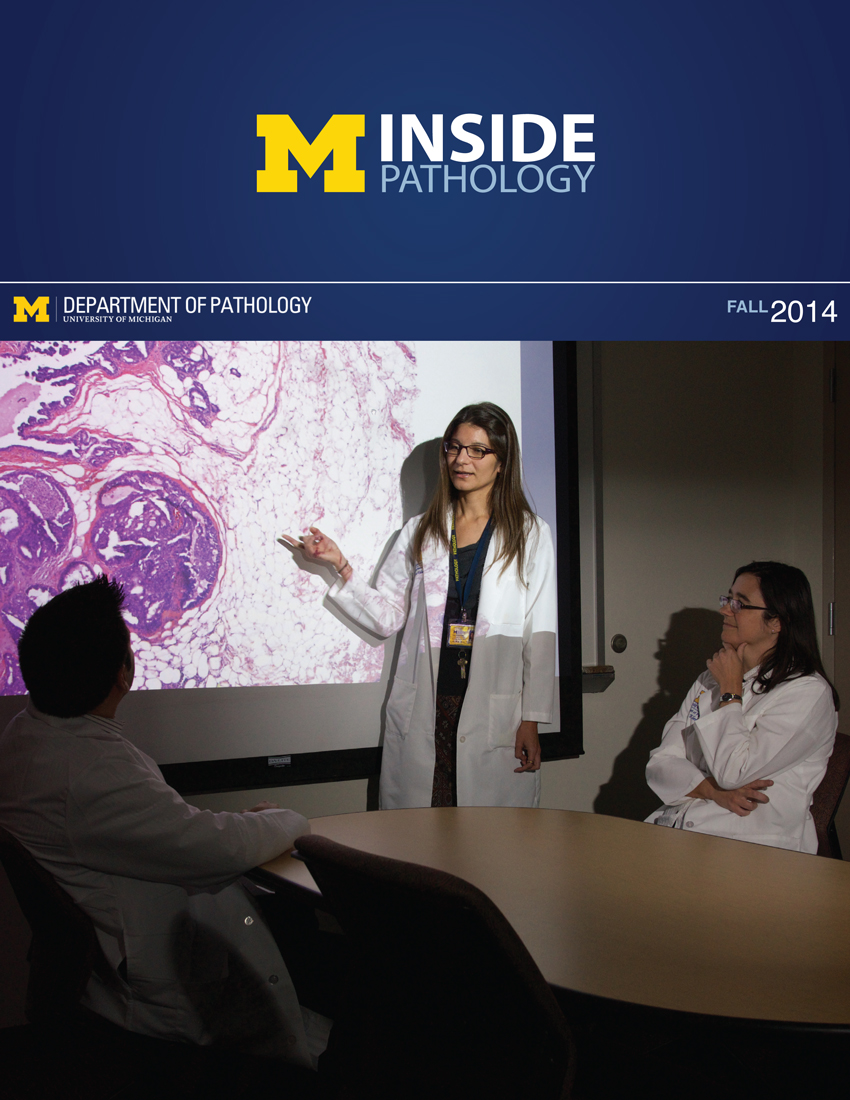 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
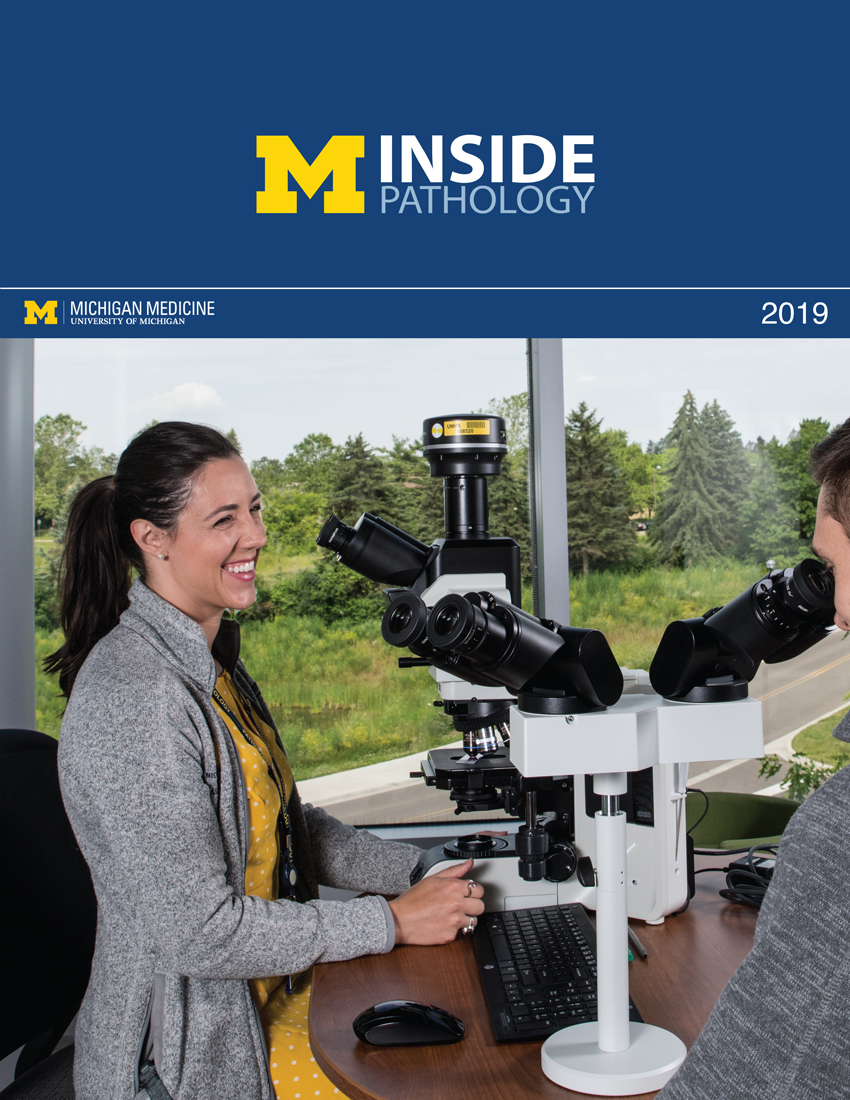 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
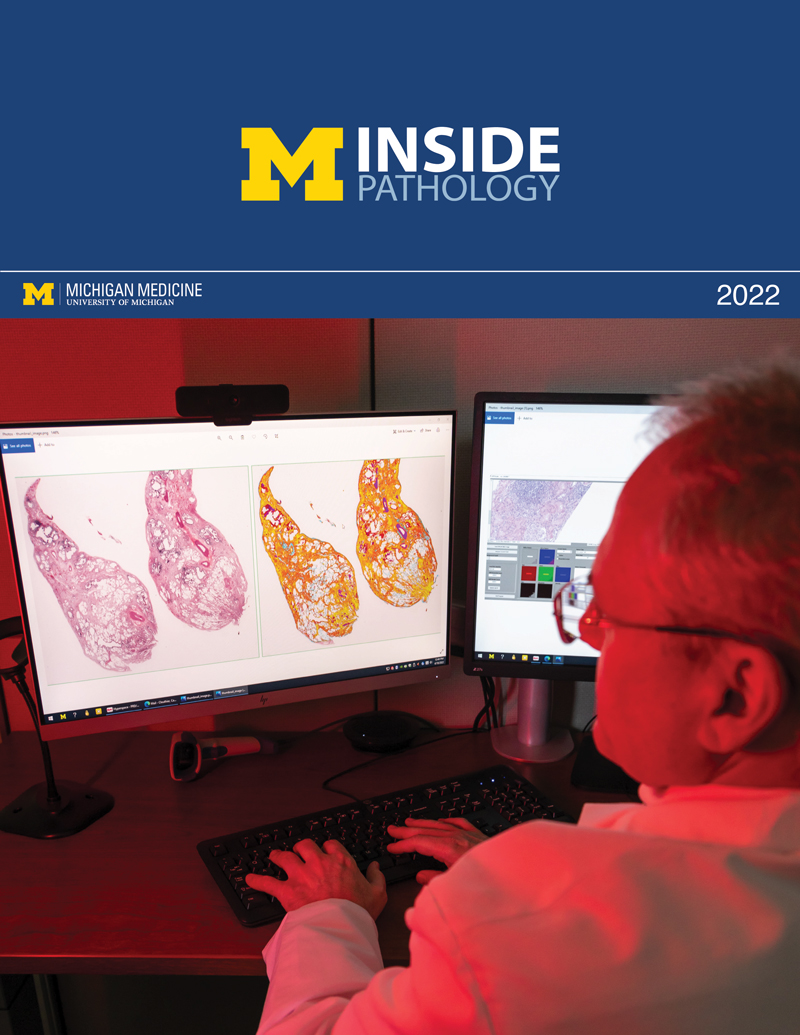 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
