Lungs of the Living
By Lynn McCain | November 23 2021Throughout the ongoing pandemic, many patients who die from COVID-19 pneumonia are found at autopsy to have a pattern of fibrosis in their lungs that resemble nonspecific interstitial pneumonia (NSIP). However, members of the Anatomic Pathology Division of Pathology at Michigan Medicine were curious about the lungs of those who survive COVID-19 pneumonia. This team is made up of Drs. Kristine Konopka, William Perry, Tao Huang, Carol Farver, and Jeffrey Myers, searched the literature and could not find any published studies looking at the lungs of living patients other than a few that examined lung transplant specimens, which showed NSIP-like fibrosis and sometimes persistent acute lung injury (ALI).
The study team queried the pathology database and pulled slides referred to our consultation service from non-Michigan Medicine patients who underwent surgical lung biopsies between January 2020 and April 2021 for persistent interstitial lung disease following recovery from COVID-19. The slides were independently reviewed by two thoracic pathologists, who were blinded to the patients’ data. The results of this study were just published online in EClinicalMedicine, a journal that is part of the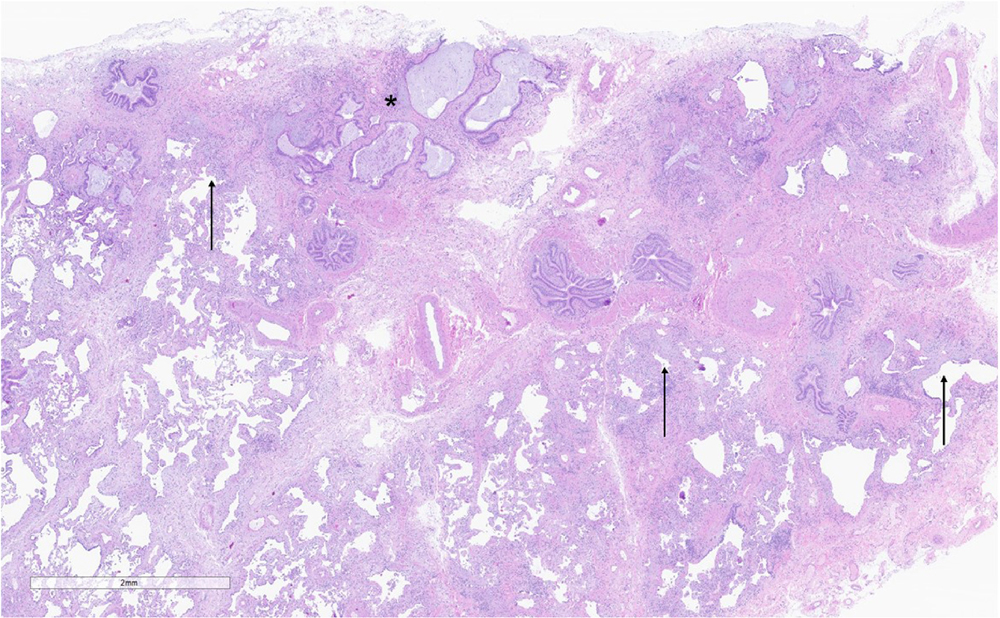 Lancet family. Of the eighteen patient cases reviewed, nine were found to have usual interstitial pneumonia (UIP). UIP is a form of progressive fibrotic lung disease that is characterized by scarring (fibrosis) of both lungs involving the supporting framework of the lung, called the pulmonary interstitium. Of these nine patients, two also had ALI. As reported in their recent publication, five cases showed a spectrum of ALI that ranged from persistent diffuse alveolar damage to organizing pneumonia. Four patients had either other less common forms of diffuse lung disease or no histopathologic findings that explained their respiratory symptoms and/or radiological findings.
Lancet family. Of the eighteen patient cases reviewed, nine were found to have usual interstitial pneumonia (UIP). UIP is a form of progressive fibrotic lung disease that is characterized by scarring (fibrosis) of both lungs involving the supporting framework of the lung, called the pulmonary interstitium. Of these nine patients, two also had ALI. As reported in their recent publication, five cases showed a spectrum of ALI that ranged from persistent diffuse alveolar damage to organizing pneumonia. Four patients had either other less common forms of diffuse lung disease or no histopathologic findings that explained their respiratory symptoms and/or radiological findings.
The study concludes, “UIP was the most common pathologic finding in patients undergoing evaluation for post-COVID-19 ILD. Our preliminary data suggest that CT changes described as an interstitial thickening, peripheral reticulations, and/or bronchiectasis may be helpful in identifying patients with underlying fibrotic chronic interstitial pneumonia for which UIP is the chief concern.”
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
