Dr. Khatri et al. Published in the Journal of the American Academy of Dermatology
By Elizabeth Walker | June 28 2018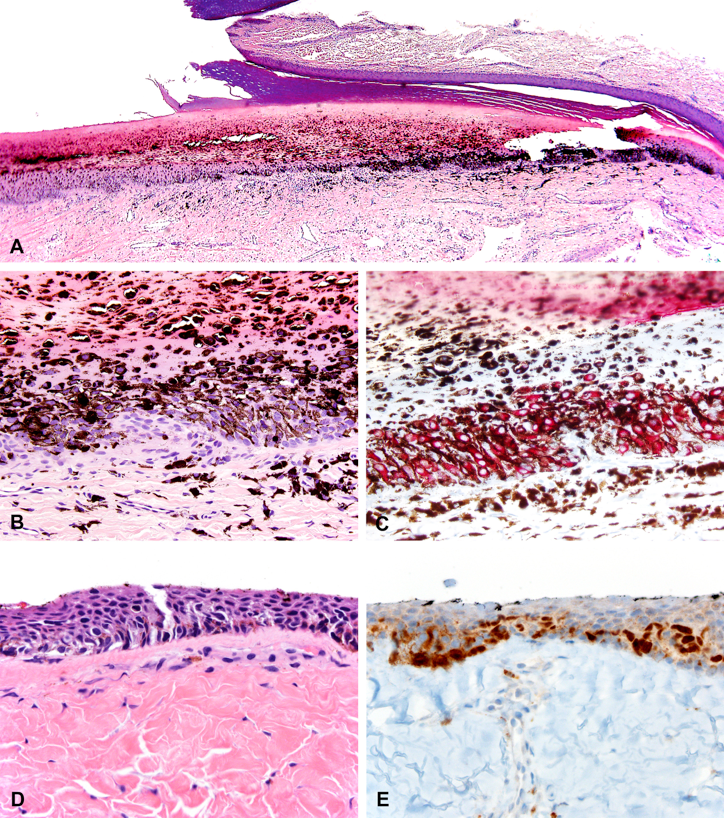 Histopathologic features of cases diagnosed as subungual melanoma in situ. A-C, Case 7. A, Scanning magnification shows a poorly circumscribed and heavily pigmented lesion involving the nail matrix epithelium. B, Atypical melanocytes are epithelioid to dendritic with large atypical nuclei, profoundly obscured by abundant melanin pigment. C, Melan-A immunostain supports confluent growth and pagetoid scatter. D and E, Case 9. D, Prominent lentiginous and pagetoid growth of atypical melanocytes with enlarged, hyperchromatic, and angulated nuclei. E, Atypical melanocytic nuclei are highlighted by MiTF immunostain. (A, B, and D, Hematoxylin-eosin stain; C, Melan-A stain; E, MiTF stain; original magnifications: A, ×20; B-E, ×400.)Dr. Dr. Sameer Khatri along with the Department of Pathology's Drs. Min Wang, Paul Harms, Douglas Fullen, Aleodor Andea, and May Chan, in collaboration with other U-M and extramural colleagues, have published the paper, Subungual Atypical Lentiginous Melanocytic Proliferations in Children and Adolescents: A Clinicopathologic Study, in the Journal of the American Academy of Dermatology (JAAD).
Histopathologic features of cases diagnosed as subungual melanoma in situ. A-C, Case 7. A, Scanning magnification shows a poorly circumscribed and heavily pigmented lesion involving the nail matrix epithelium. B, Atypical melanocytes are epithelioid to dendritic with large atypical nuclei, profoundly obscured by abundant melanin pigment. C, Melan-A immunostain supports confluent growth and pagetoid scatter. D and E, Case 9. D, Prominent lentiginous and pagetoid growth of atypical melanocytes with enlarged, hyperchromatic, and angulated nuclei. E, Atypical melanocytic nuclei are highlighted by MiTF immunostain. (A, B, and D, Hematoxylin-eosin stain; C, Melan-A stain; E, MiTF stain; original magnifications: A, ×20; B-E, ×400.)Dr. Dr. Sameer Khatri along with the Department of Pathology's Drs. Min Wang, Paul Harms, Douglas Fullen, Aleodor Andea, and May Chan, in collaboration with other U-M and extramural colleagues, have published the paper, Subungual Atypical Lentiginous Melanocytic Proliferations in Children and Adolescents: A Clinicopathologic Study, in the Journal of the American Academy of Dermatology (JAAD).
Melanonychia, characterized by longitudinal pigmented streak or diffuse pigmentation of the nail plate, may be caused by benign or malignant melanocytic proliferation among other etiologies. Atypical subungual melanocytic proliferations are rare in children and adolescents but often present a significant diagnostic challenge to dermatopathologists, in part owing to limited experience. Khatri et al. reported 11 subungual atypical lentiginous melanocytic proliferations occurring in pediatric patients, all of which demonstrated some degree of clinical atypia and histologic features indistinguishable from adult subungual melanoma in situ.
Fluorescence in situ hybridization (FISH) using a melanoma probe set was positive in 1 of 4 tested cases. Three lesions recurred without further adverse outcome. The study concluded that routine histopathology does not predict molecular abnormalities or recurrence. Given the rarity of reported adverse outcome in the literature and in this cohort, it was recommended that clinicians maintain a high threshold for biopsy while closely monitoring melanonychia in pediatric patients. Once a subungual atypical lentiginous melanocytic proliferation is diagnosed on biopsy, FISH might aid in risk stratification. Awareness of this rare group of lesions is crucial for facilitating future investigation into its biologic behavior.
—
To read the paper in its entirety, visit the JAAD.
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
