Research Led by Dr. Udager Published in Modern Pathology
By Camren Clouthier | November 19 2020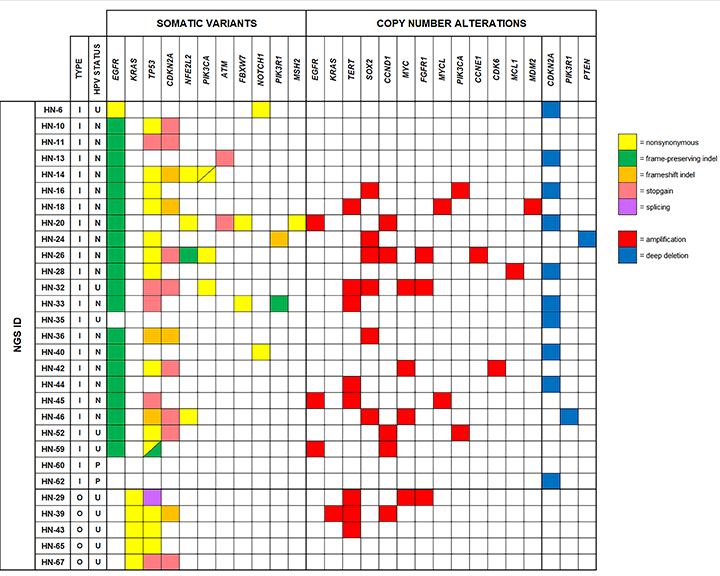 New research by the Department of Pathology was recently published in Modern Pathology. The study, led by Drs. Aaron Udager, Noah Brown, Bryan Betz, Jonathan McHugh, and Scott Tomlins, focuses on how TP53 mutations and CDKN2A mutations and deletions are highly recurrent molecular alterations within the malignant progression of sinonasal papillomas.
New research by the Department of Pathology was recently published in Modern Pathology. The study, led by Drs. Aaron Udager, Noah Brown, Bryan Betz, Jonathan McHugh, and Scott Tomlins, focuses on how TP53 mutations and CDKN2A mutations and deletions are highly recurrent molecular alterations within the malignant progression of sinonasal papillomas.
Initially, experts theorized that sinonasal papillomas are benign epithelial tumors of the sinonasal tract that are associated with a synchronous or metachronous carcinoma in a subset of cases. The research team recently identified mutually exclusive EGFR mutations and human papillomavirus (HPV) infection in inverted papillomas and frequent KRAS mutations in oncocytic papillomas. The team also demonstrated concordant mutational and HPV infection status in sinonasal papilloma-associated carcinomas, confirming a clonal relationship between these tumors. Despite an emerging understanding of the oncogenic mechanisms driving the formation of sinonasal papillomas, little is currently known about the molecular mechanisms of malignant progression to cancer. However, in the present study, experts utilized targeted next-generation DNA sequencing to characterize the molecular landscape of a large cohort of sinonasal papilloma-associated carcinomas.
 According to Dr. Udager, "using targeted next-generation DNA sequencing, we have demonstrated that sinonasal papilloma-associated carcinomas have several unique molecular features that differentiate them from other aerodigestive tract squamous cell carcinomas. We have established that TP53 mutations and/or CDKN2A mutations/deletions are central molecular events in the malignant progression of sinonasal papillomas."
According to Dr. Udager, "using targeted next-generation DNA sequencing, we have demonstrated that sinonasal papilloma-associated carcinomas have several unique molecular features that differentiate them from other aerodigestive tract squamous cell carcinomas. We have established that TP53 mutations and/or CDKN2A mutations/deletions are central molecular events in the malignant progression of sinonasal papillomas."
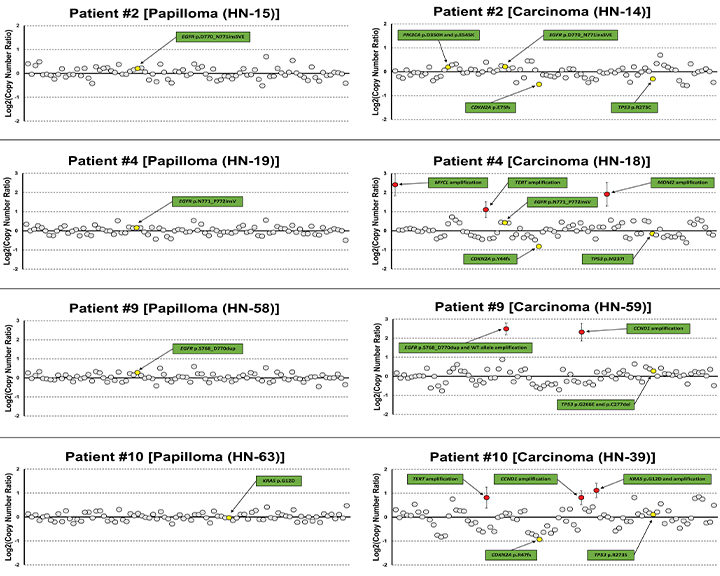
As expected, EGFR or KRAS mutations were present in the vast majority of tumors. In addition, highly recurrent TP53 mutations, CDKN2A mutations, and/or CDKN2A copy-number losses were detected. Overall, nearly all tumors harbored at least one TP53 or CDKN2A alteration. TERT copy-number gains also occurred frequently; however, no TERT promoter mutations were identified. Other recurrent molecular alterations included NFE2L2 and PIK3CA mutations and SOX2, CCND1, MYC, FGFR1, and EGFR copy-number gains. Importantly, TP53 mutations and CDKN2A alterations were not detected in matched papillomas, suggesting that these molecular events are associated with malignant transformation.
 Compared to other aerodigestive tract squamous cell carcinomas from The Cancer Genome Atlas (TCGA) project, sinonasal papilloma-associated carcinomas have a distinct molecular phenotype, including more frequent EGFR, KRAS, and CDKN2A mutations, TERT copy-number gains, and low-risk human papillomavirus (HPV) infection.
Compared to other aerodigestive tract squamous cell carcinomas from The Cancer Genome Atlas (TCGA) project, sinonasal papilloma-associated carcinomas have a distinct molecular phenotype, including more frequent EGFR, KRAS, and CDKN2A mutations, TERT copy-number gains, and low-risk human papillomavirus (HPV) infection.
Ultimately, these findings shed light on the molecular mechanisms of malignant progression of sinonasal papillomas and may have important diagnostic and therapeutic implications for patients with advance forms of cancer. "This work builds upon prior seminal research from our group over the past five years that have defined the major molecular oncogenic drivers in sinonasal papillomas, and ongoing work in my laboratory is focused on translating these molecular insights into new tests and/or therapeutic options for patients with sinonasal papillomas and associated carcinomas,” notes Udager.
—
The full publication in Modern Pathology is available here.
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
